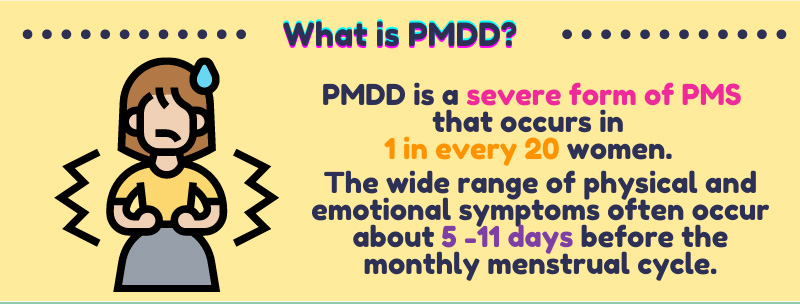
PMDD is a severe form of PMS that is experienced by 1 in 20 women worldwide. It is often known for painful symptoms such as headaches, pelvic pain, bloating, breast tenderness, irritability, depressed mood, tension, and fatigue. Even though many women experience this every month, not much is known about this disorder, especially what causes it. Women are then usually left to manage the symptoms instead of the condition itself.
In 2016, a group of Swedish researchers investigated the possible cause of PMDD. The purpose of their study was to examine potential qualitative and quantitative differences in brain serotonin activity among women suffering from PMDD.
Previous studies by Perach-Barzilay N., et al. (2013) and Yang Y. et al. (2009) have found that the dorsolateral prefrontal cortex plays an essential role in dealing with impulse and aggression control. Another research by Hecht D. (2013) and Abbott J. et al. (2013) has shown that, to a great extent, negative emotions are primarily under the control of the right hemisphere of the brain. These three symptoms, impulse, aggression, and generally negative emotions such as depression and irritability, are characteristics of PMD.
The study by Eriksson et al. (2016) involved twenty women: 12 are suffering from PMD, and 8 have no premenstrual mood symptoms to serve as the control.

During the study, the subjects were asked to evaluate their symptoms, including mood variables and physical health symptoms. Specifically, the evaluation included mood variables: irritability, depressed mood, happiness, relaxation, and friendliness. On the other hand, the physical health variables are energy, tension, fatigue, headache, pelvic pain, bloating, breast tenderness, sexual desire, and craving for sweets. Aside from self-evaluation, the study also used a positron emission tomography (PET) scan of the brain during mid follicular (postmenstrual) and late luteal or (premenstrual) phases of their cycles.
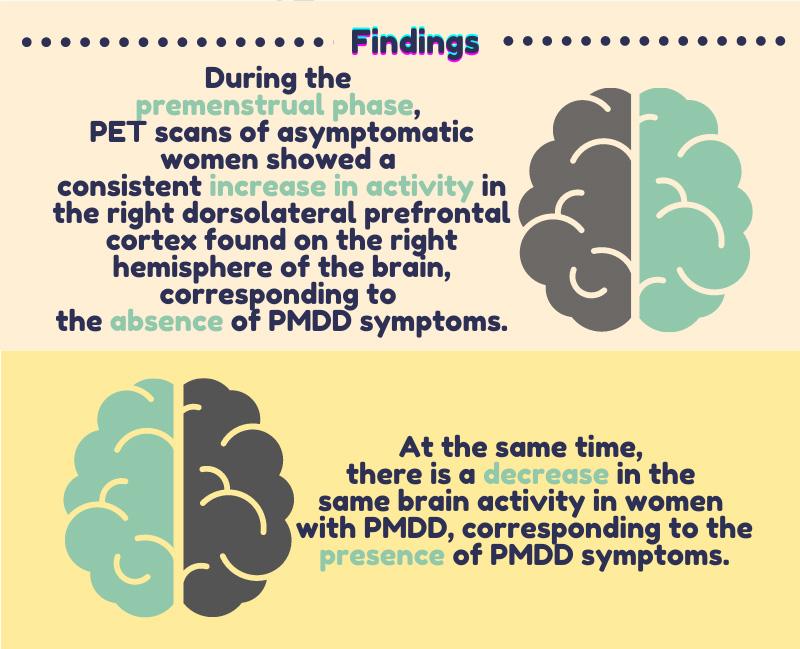
Eriksson, O. et al. (2016) found a significant and noticeable difference between the dorsolateral prefrontal cortex activity during the premenstrual phase of asymptomatic subjects. Results showed a consistent increase in premenstrual brain activity in the right dorsolateral prefrontal cortex in the asymptomatic group. At the same time, there is a decrease in the same brain activity in women with PMD. This pattern observed in asymptomatic women corresponded to the absence of symptoms of PMD, while the reverse pattern in patients with PMD corresponded to the presence of PMD symptoms.
Their key findings imply that women who do not experience PMD symptoms have an innate capability to increase their relative serotonin activity on the right side of the dorsolateral prefrontal cortex during the premenstrual phase of their cycle. This increase in serotonin activity possibly lessens the negative emotions and symptoms experienced during this part of the menstrual cycle. On the other hand, the study also implies that women who suffer from PMD do not have the same intrinsic means of increasing their serotonin activity to dampen the symptoms of PMD.
A possible future application of this study is the use of antidepressants, specifically Selective Serotonin Reuptake Inhibitors (SSRIs), to regulate the symptoms of PMD. SSRIs work by increasing the neurotransmitter serotonin level, also known as the ‘feel-good’ hormone.
This study is a step towards a better understanding of female reproductive and mental health. In the future, it could be possible that modern women will not have to suffer through painful symptoms every month and would tackle their premenstrual dysphoria disorder head-on.
References:
Eriksson, O., Wall, A., Olsson, U., Marteinsdottir, I., Holstad, M., Ågren, H., Hartvig, P., Långström, B., & Naessén, T. (2016). Women with Premenstrual Dysphoria Lack the Seemingly Normal Premenstrual Right-Sided Relative Dominance of 5-HTP-Derived Serotonergic Activity in the Dorsolateral Prefrontal Cortices – A Possible Cause of Disabling Mood Symptoms. PloS one, 11(9), e0159538. https://doi.org/10.1371/journal.pone.0159538
Perach-Barzilay, N., Tauber, A., Klein, E., Chistyakov, A., Ne’eman, R., & Shamay-Tsoory, S. G. (2013). Asymmetry in the dorsolateral prefrontal cortex and aggressive behavior: a continuous theta-burst magnetic stimulation study. Social neuroscience, 8(2), 178–188. https://doi.org/10.1080/17470919.2012.720602
Yang, Y., & Raine, A. (2009). Prefrontal structural and functional brain imaging findings in antisocial, violent, and psychopathic individuals: a meta-analysis. Psychiatry research, 174(2), 81–88. https://doi.org/10.1016/j.pscychresns.2009.03.012
Hecht D. (2013). The neural basis of optimism and pessimism. Experimental neurobiology, 22(3), 173–199. https://doi.org/10.5607/en.2013.22.3.173
Abbott, J. D., Cumming, G., Fidler, F., & Lindell, A. K. (2013). The perception of positive and negative facial expressions in unilateral brain-damaged patients: A meta-analysis. Laterality, 18(4), 437–459. https://doi.org/10.1080/1357650X.2012.703206