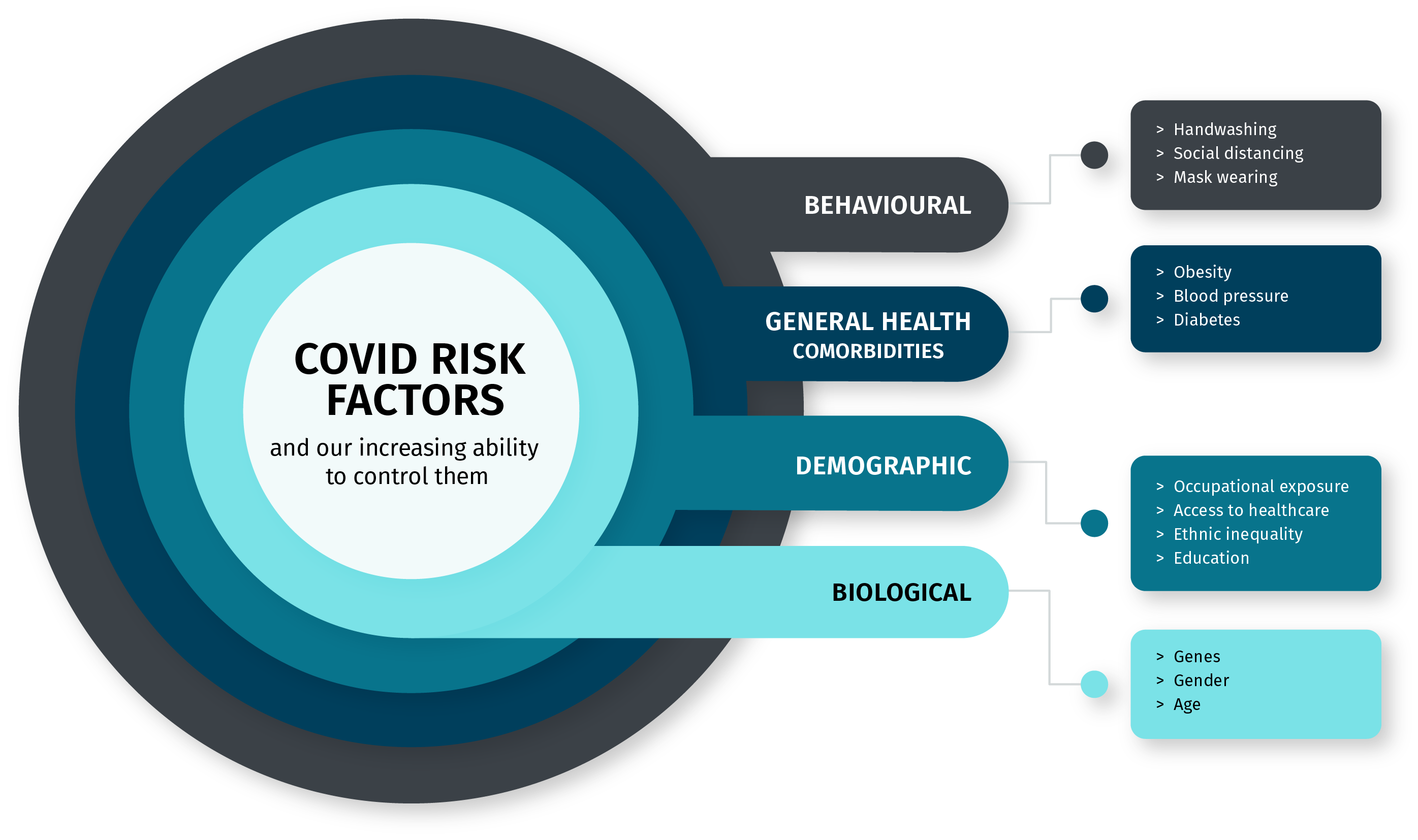
Risk factors impacting your susceptibility to COVID-19 & your ability to control them. Credit: Molly Patton
Author: Manisha Roy
Feature Image Designer: Molly Patton
Robin Cook’s movie-adapted book ‘Contagion‘ came to life with an invisible disaster striking Earth and switching the whole world into panic mode. In an experience of a lifetime, the world came to a standstill for months together during the ‘Great Lockdown’.
Slowly, as we approach year-end, there looks to be no sign of relief from SARS-CoV-2. For a quick reminder, this unwanted guest dropped itself into the human population at the onset of this year. Ugh! Reminds me of an annoying guest who overstays their welcome.
As of October 16, globally around 39 million individuals have been tested positive for COVID-19 and 1.1 million people have lost their lives. During its early outbreak, in a movie reel-turns-real scenario, the globe faced multiple back-to-back lockdowns both long and short, work-from-home schedules, shortages of groceries and vegetables, empty streets and roads, and most importantly a constant fear of COVID-19 lurking outside. Ten months on and it continues to spread its way across the planet.
Now, as we come to terms with the world post-pandemic outbreak, we are adjusting our lives to their new normal. While restrictions are being eased in some countries (e.g. Australia & New Zealand), it is not yet safe to venture outside in other parts of the world without appropriate safety measures and practices.
COVID-19 can infect anybody who comes in contact with it, but there is a particular subset of the population that is more prone to a fatal or near-fatal rendezvous with this unwanted guest. Through this article, we will attempt to disentangle the confusion around COVID-19 risk factors, both demographic, behavioral and biological. There are various factors which have been unknown to us until recently. We have listed the most important and proven ones for you here.
AGE
Age plays a leading role in determining the severity of the illness due to COVID-19. As we age our immune system weakens, making us more prone to infectious diseases. And with few safe and efficacious treatments available for COVID-19 today, it is difficult to curb its spread within the body. Additionally, the elderly population tends to have a bevy of one or more long-term health issues, which may explain excess fatalities in the older age group.
An early COVID-19 pandemic study in the U.S. showed that the fatality rate was highest in persons:
- aged ≥85 years (range 10%–27%), followed by
- aged 65-84 years (3%–11%), followed by
- aged 55-64 years (1%–3%), followed by
- aged <55 years (<1%)
COMORBIDITIES
High blood pressure, diabetes, respiratory diseases and obesity are the most dominant risk factors for a severe infection and fatality from COVID-19. These health conditions can increase the chances of COVID-19-related hospitalization and critical care. Furthermore, individuals with prior heart attacks, strokes and kidney disease also run a risk of negative outcomes from COVID-19 infection. These conditions may give rise to chronic low-grade inflammation, hence compromising our immune system and enabling an easy security breach by pathogens.
Lung tissues are the prime location of attack for SARS-CoV-2, which is primarily a respiratory infection. Some complications, like blood clots, stroke, renal failure and cardiac failure can also arise as the virus enters organs other than lungs.
In addition, underlying health conditions can affect your metabolism and make it easier for bacteria and viruses (such as SARS-COV-2) to enter your bodily system. Certain infections can also interfere with hormonal production in the body, making it all the more difficult for your system to generate a neck-to-neck battle with the virus.
GENDER
COVID-19 hits males harder than females. Well established data now shows that men are more likely to become seriously ill from coronavirus than females. The answer could lie in higher rates of smoking, diabetes, hypertension and high blood pressure in men than in women, which may escalate the chances of complications following an infection in men. Another possible reason lies in a stronger immune system among women. Women fare better at fighting infectious diseases than men. The presence of an extra X chromosome, which carries genes associated with important immunity-boosting entities, may make this possible.
“It turns out that there are over 60 genes associated with immune function on the X chromosome,” Dr. Sabra Klein has said. She is a molecular biologist and co-director of the Johns Hopkins Center for Women’s Health, Sex, and Gender Research. “My group and others have shown that females show greater expression of some of these genes than do males,” Klein added, “and this can have functional significance.”
“It turns out that there are over 60 genes associated with immune function on the X chromosome [carried by all women]” – Dr. Sabra Klein, Johns Hopkins Bloomberg School of Public Health
YOUR GENES
Deep down inside, everybody on this planet varies from each other biologically (except for identical twins!). The reason lies in our genetic makeup, i.e. the way our body is made up, the building blocks of our body. The ability of our body to fight against a host of illnesses is influenced, to a great extent, by genes involved in structuring the immune system. Certain genes, or alterations in the gene, might make a person more vulnerable to sickness, while others may confer resistance. This explains why some people can fight an infectious disease like COVID-19 more firmly while others can’t. Therefore, every individual’s risk category is different.
For instance, there are reports that suggest the quantity of expression of angiotensin-converting enzyme 2 or ACE2 receptors in an individual is an aggravating factor for COVID-19. ACE2 is present on the surface of the majority of our cell types. It helps the virus gain entry into a cell and is present in varying numbers in different individuals based on various genetics and environmental factors. However, its role is yet to be fully understood.
Other than that, there are blood type determining genes that put an individual at a higher risk of a serious COVID-19 infection. For example, individuals with blood group ‘A’ are at higher risk than others. Similarly, those with type blood type ‘O’ are at lower risk of severe illness due to COVID-19.
SOCIETAL FACTORS
Though it is not fully understood, there are reports of people of certain racial and ethnic minority communities being disproportionately affected by COVID-19. It appears unlikely that there is a biological factor behind the differences in rates of severe illness or death. Economic vulnerability, inaccessibility to healthcare facilities, quality education and inequalities are some of the causes behind different outcomes from COVID-19.
“Race doesn’t put you at higher risk. Racism puts you at higher risk,” Dr. Camara Phyllis Jones has said. She is a social epidemiologist at the Morehouse School of Medicine and ex-president of the American Public Health Association. “Racism puts you at higher risk through the two mechanisms of being more infected because we are more exposed and less protected, and then, once infected, we are more likely to have a very severe course and die,” she added.
Occupation exposure is one of the factors behind the high infection rate in individuals from minority ethnic groups. For instance, those working in healthcare or social care come in contact with several people in a day. This increases the risk of falling sick with COVID-19. Apart from this, the inability to get paid sick leave, lack of work from home options, and insufficient savings add to the burden. Stress caused by unfortunate incidents of unemployment or unexpected expulsion from jobs multiplies the risk of infection.
Some groups share housing or lead a life in crowded conditions where it is difficult to maintain social distancing or self-isolation. Due to these reasons, people of racial and minority ethnic origin are more prone to becoming seriously ill from coronavirus.
The aforementioned circumstances might be the reason behind more people of ethnic minority background being affected by COVID-19. That being said, these factors do not affect all individuals of a community as a general rule.
LIFE WITH COVID-19
As of now, there is not much concrete knowledge about the NOVEL coronavirus – The name says it all. Most of the present knowledge comes from its siblings SARS and MERS. Years might pass on trying to comprehend it. With no vaccine around, until then taking precautions is the best approach.
There is an array of other factors, beyond the length-and-breadth of this article, which may prove to be significant, as more and more research is taken up.
Whether or not one falls in a high-risk category, one needs to take utmost precaution relating to contracting or spreading COVID19. People of the younger age group are also falling victim to COVID-19. Wearing a mask, frequent and thorough handwashing, particularly before eating food, social distancing helps in lowering the risk of contracting and spreading COVID-infected droplets and lowers the risk for everyone, especially the most vulnerable.